Drug Abuse and My Own Biased Compassion
Stigma and sterotypes inside the treatment arena.
It's bad enough when substance misusing clients run into stigma, bias, prejudice and stereotyping as they try to navigate their life paths forward in recovery. It's much worse when they receive poor treatment, or are refused treatment, within the medical and mental health arena itself, the very places that they look to for acceptance and care. Unfortunately, many clients are refused treatment because they present with addiction, while others receive poor treatment that can appear rote or even adversarial.
Those of us in the professional treatment community are all-too-familiar with the stigmatization that our substance misusing clients face with regards to employment, housing and many other aspects of society. What is less frequently commented upon is the conscious or unconscious bias towards substance misusers that our clients, and we as (almost) professionals in the nursing field, encounter from within the medical and psychiatric establishment.
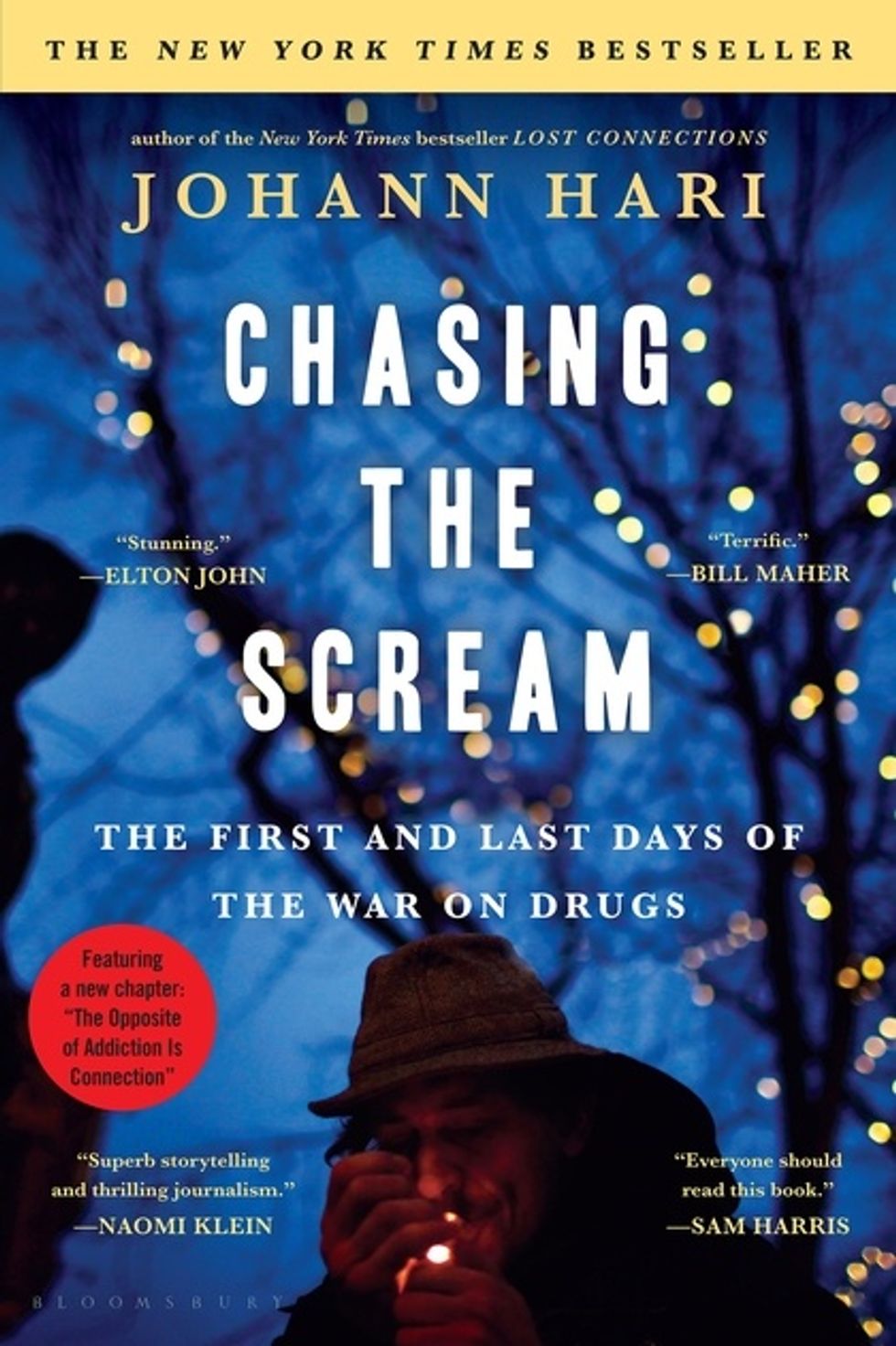
Sadly, such bias toward substance misusers is a common part of working in the field of addiction. Many refuse to treat substance misusers, whose situations can seem too challenging, and often come with lots of complications including medical problems, personality disorders, family conflicts and legal issues. "Old school" thinking that addiction is somehow a moral failing rather than a complex biopsychosocial disorder is still prevalent. Some worry about prescribing or administering medication that will end up diverted or abused by the patient. Health professionals who refuse to work with substance abusers stereotypically see them as deceptive and prefer to work with individuals who do not present such challenges. Many social workers and therapists will only work with patients who are abstinent—claiming that substance use renders mental health treatment less effective or ineffective.
I even battle with my own bias, both conscious and unconscious. After spending a day during one of my clinical rotations with a young IV drug user, I came away convinced that she was not truly interested in changing. She told me how she got into drugs and was homeless, and about all the damage she had done to her family by getting arrested and stealing. I thought my chances of helping this lady were slim to none, because she was clearly not invested in helping herself. I felt myself shutdown and my suspicions rise up. I realized I had to take a step back and examine my countertransference and get a grip on my prejudicial thinking. Was it her nonchalance in telling her story that biased me against her, perhaps just from her telling her story to countless other nursing students? Was it her skinny, disheveled appearance? Was it her repeated requests for assistance and pain medication? Was it my own feelings of hopelessness in the face of how to help this very troubled individual? After discussing this case with a colleague, I became clear about the path I needed to take. This young woman was coming for help and despite her history and presentation, I had to put aside my bias and give her a chance, even if just in my own mind.
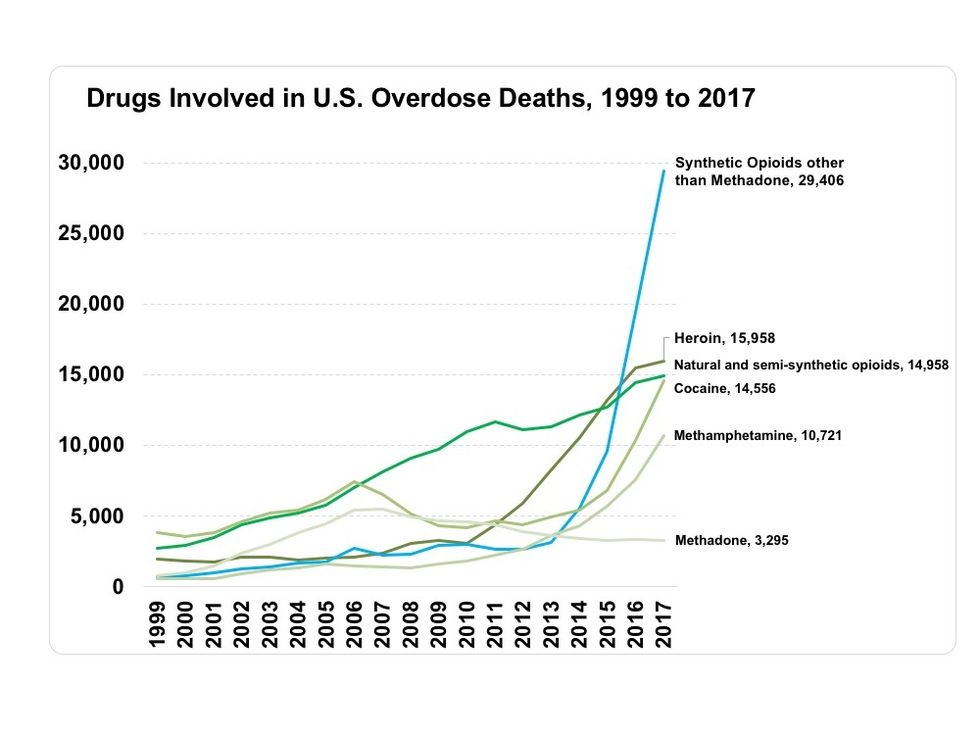
We all fall prey to stereotypes and prejudices. Treating substance misusers is challenging work, and many of the concerns that health professionals have regarding working with them are often valid. We are human beings with messy insides, and we need to be aware and vigilant of what happens internally as we treat this population. The insights and experience of otherswho work in addiction are extremely valuable in battling one's own bias in treating addiction. With substance use on the rise, more and more health professionals will be faced with patients in their hospital rooms who initially present with depression or anxiety but then reveal a co-existing alcohol or drug problem. Hopefully, we as professionals will be able to battle our biases, roll up our sleeves…and help.



 via google
via google